UW Research: Grace Grants
2024 Grace Grant: A Resurgence of JAK/STAT Signaling in Chronic Epilepsy
Epilepsy is the 4th most common brain disorder, affecting 1 in 26 people. There are no treatments in existence for epilepsy patients that stop seizures, restore normal brain function, and provide enduring protection against seizures after drug is withdrawn. Such a treatment is called “disease modification,” and it is the holy grail of epilepsy research.
Currently, all experimental interventions to prevent acquired epilepsy focus on manipulations either prior to brain insult, or early after initial insult, before manifestation of spontaneous seizures i.e. before epilepsy. However, none of these approaches are available to patients because patients cannot be treated prior to injury, exceptionally few patients know when they’ve had an epileptic insult, and most often patients appear in the clinic already having epilepsy. We have identified a specific target and mechanism that can be used to completely silence seizures and restore normal brain function once epilepsy has been diagnosed. This is a world-first. By comparing gene changes in the brains of epileptic rodents and human brain tissue, we have found that a molecular pathway called JAK/STAT3 is rapidly turned on with epileptic insults but quickly disappears within days.
Many other labs have reported this and all have tried to intervene during this early period to try and stop epilepsy from developing. All attempts to curtail this pathway in a clinically relevant manner have failed. However, Dr. Avtar Roopra and his lab have discovered that the pathway reignites weeks later when the brain becomes epileptic. We have discovered that this new, resurgent activation can be targeted with CP690550, an FDA approved drug for other diseases. CP690550 (tofactinib/Xeljanz), when given for a 2-week window to already-epileptic mice, silences seizures for at least a month after the last dose of the drug and restores normal brain function. This grant will explore the extent of protection of this disease modifying agent.
2024 Grace Grant: Mapping Neural Network Dynamics Underlying Epilepsy in Children
2022 Grace Grant: The Effects of Infant Diet
During our first year of Grace Grant funding, we asked parents of children with Dravet syndrome to complete an online survey that collected data on what they fed their children when they were infants as well as seizure history and other comorbid disorders. Our primary goal was to determine if infants with Dravet syndrome who were fed a soy-based infant formula had more seizures and worse comorbidities than infants fed breast milk or cow milk-based infant formula.
We had 31 parents complete the survey and we are currently analyzing the data. We also performed complementary experiments in a mouse model of Dravet syndrome where we fed Dravet mice and wild type littermate controls common rodent chows versus refined diets containing soy versus casein protein. Then we tested a wide range of behaviors including seizures, hyperactivity, autism, motor coordination, and learning and memory in response to the different diets. We tested over 150 mice in the behavior panel and then collected blood samples from the animals to measure the levels of dietary chemicals in the blood. We are in the process of doing statistics on the data. A staff scientist, several undergraduate students, and a high school student participated in the project. We believe this type of cross-disciplinary research in neuroscience and nutrition will help us understand environmental factors that exacerbate epilepsy as well as lead to dietary interventions that reduce seizure severity in Dravet syndrome and other epilepsy-related disorders.
2021 Grace Grant: Understanding Ion Channels
Many cases of epilepsy are caused by mutations in ion channels, called ion channel variants. Ion channels cause neurons to fire, and variants that change their function may lead to seizures. It often takes years to find medications that stop seizures caused by ion channel variants. Multiscale computer models are valuable tools that represent the function of the brain on several different levels and can predict the effects of changes in ion channel function. With support from Lily’s Fund, Dr. Andrew Knox will test ion channel variants in the lab and then use a multiscale computer model to predict whether ion channel variants lead to seizures, and which medications stop seizures for each different variant. These studies will further our understanding of how ion channel variants lead to seizures. More importantly, they will lay the groundwork for future clinical studies that use genetic profiles to predict medications that will stop seizures.
We used a computer model to study how changes in ion channels (the cellular machines that cause neurons to fire) lead to seizures. Computer simulations showed that many changes in different ion channels can cause both epileptiform discharges (markers of epilepsy) and seizure activity that never stops (epileptic encephalopathy). We also found that changes in ion channels alone are not enough to cause seizure that start and stop. We found that certain patterns of firing and changes in concentration of chloride were important for reproducing seizures that start and stop like the seizure seen in most patient with epilepsy. The final version of this computer model will be an essential tool to test the effects of antiseizure medications or cortical stimulation for patients with genetic changes affecting ion channels (like Dravet Syndrome).
We also studied 13 SCN1A variants (the gene that codes for the ion channel implicated in Dravet syndrome) identified in children with epilepsy seen in the UW Health clinic. For many of these variants, it was not clear whether they caused epilepsy from the genetic change alone. Our collaborators at Northwestern used high throughput patch clamp testing performed in the lab to show that the genetic variants affected channel function in 12 of 13 patients. Finally, computer modeling showed that all of these changes in channel function lead to depolarization block, a state where inhibitory neurons (neurons that fire to quiet down other neurons) can’t fire, leading to seizures. This work may provide a new treatment target for patients with Dravet syndrome.
Over the last 9 months, we have finished adapting our multiscale computer model to incorporate experimental data describing variant sodium channels. We have collected detailed clinical data (seizure history, developmental history and neuropsychology testing, EEG data, genetic data) for 11 children with SCN1A variants. Although delayed by COVID, our collaborator Dr. Alfred George at Northwestern University, is just completing studies to characterize the function of these variants using high-throughput patch clamp. We are excited to incorporate these data into the computer model to study their network-level effects!
2020 Grace Grant: Is it Possible to Predict and Prevent SUDEP?
For most people, sleep is a time for the brain to rest and recharge. But what happens to people who live with epilepsy during sleep? And what brings on Sudden Unexpected Death in Epilepsy — aka SUDEP?
Assistant Professor of Neurology Dr. Melanie Boly, MD, PhD, is pursuing a theory. In her previous research using high-density EEG (HD-EEG) technology, Melanie has shown that brain activity in patients with epilepsy is different during sleep than those who don’t have epilepsy. There is an increase in slow-wave activity that correlates to recent seizures. She believes this activity is altering the brain in ways that affect the autonomic nervous system, which regulates things like heart rate and breathing. This, she posits, may eventually result in SUDEP.
With a $100,000 Grace Grant from Lily’s Fund, Melanie has set out to achieve two goals. First, using HD-EEG, determine if there are markers that show an increase in neuron excitability. Second, find out if this correlates with instability in heart rate, respiratory rate, and other autonomic function.
Everyone knows that SUDEP is a serious threat for patients with epilepsy. Nobody knows its root cause or how to identify at-risk patients. Melanie’s research has the potential to identify new diagnostic tools to identify patients who are at high risk of SUDEP. Ultimately, this will pave the way for new therapeutic interventions to improve the body’s regulatory systems during sleep to prevent SUDEP.
2019 Grace Grant: Could Inflammation be at the Root of Seizures?
There is a longstanding theory in the field of epilepsy that seizures beget more seizures. What if the reason for that is simple inflammation of the brain? That’s what our newest Grace Grant recipient intends to find out.
Aaron F Struck, M.D., Assistant Professor of Neurology, will be recruiting patients at the epilepsy monitoring unit at UW to shed light on whether seizures themselves cause inflammation, and if the inflammation correlates with the region from which the seizures came. This could open the door to a wide array of treatments using anti-inflammatory drugs to blunt the effect of seizures.
Patients and families of people with epilepsy are very aware that there is gap between promising basic research about epilepsy and its impact on understanding and treatments in people. Basic science research has uncovered many of the processes underlying epilepsy in animal models though we still have little understanding if these same processes are at play in human epilepsy and how to change these findings into therapies. All of the seizure medications essentially aim at decreasing the excitability of brain cells and none at the fundamental process of epilepsy.
Struck and team want to close this gap by using molecular imaging in patients with seizures. Molecular imaging is the process of tagging molecules with a radio signal so that the biochemistry underlying epilepsy in patients can be indentfied for potential new therapeutic targets to stop seizures. The first target they will look at is inflammation. There is ample animal model data to suggest that inflammation can result in lowering of the seizure threshold as well as permanent changes to brain cells that make them more susceptible to seizures. There is human data showing that inflammation is present in seizure-producing regions. Where this inflammation comes from is unknown.
This study looks to see if seizures themselves can cause this inflammation and in turn foster the process of epilepsy, providing evidence of the longstanding theory that seizures themselves beget more seizures. The team will be using state-of-the-art neuroimaging technique [18F] FEPPA PET/MR that creates a snapshot of brain inflammation. These scans will be done twice on the same patient, once when they have been seizure free for at least 2 weeks and then again after they have had several seizures.
This data will show if seizures themselves cause inflammation and if the inflammation correlates with the region from which the seizures came, opening the door on the wide array of treatments already available to treat inflammation and creating another technique for seizure localization for surgical work-up of epilepsy patients.
Due to the pandemic, the Extended Monitoring Unit (EMU) for epilepsy patients was closed for several months. Dr. Struck’s research depends on patients to have access to PET and MRI scans. The EMU has now reopened and epilepsy patients have access to the full range of treatment and diagnostic options at this level 4 comprehensive epilepsy center. His clinical research is now resuming and recruitment has begun.
2016 Grace Grant: Effects of Sleep Deprivation
People who live with epilepsy have a wide variety of symptoms and many different kinds of seizures. Similarly, they often have many different triggers—things that can provoke seizures or make them more likely. One of the most common triggers is sleep deprivation.
Researchers, physicians, patients and families will tell you that lack of sleep can often increase the likelihood of seizures, even in patients whose epilepsy is well controlled with medication. Although this problem is well known, scientists and physicians don’t have a lot of knowledge about the relationship between sleep and seizure susceptibility. With a two-year, $100,000 Grace Grant from Lily’s Fund, Dr. Rama Maganti and Associate Professor Mathew Jones will study how sleep deprivation, acute or chronic, alters seizures. They will examine how mechanisms in the brain are altered by sleep deprivation and whether this phenomenon can be prevented.
It has been known for a long time that certain parts of the temporal lobe of the brain are a) involved in memory and b) hotspots for seizures in temporal lobe epilepsy (TLE).
One of these regions, the dentate gyrus, is involved in a very specific aspect of memory called “pattern separation”: the ability to keep straight numerous, similar memories and is thought to act as a “filter” that prevents excessive excitability.
The dentate gyrus is well-known as the site of numerous anatomical and functional disruptions in TLE. Together, this knowledge predicts that TLE should include *both* hyperexcitability in the dentate gyrus and a breakdown in pattern separation memory function.
The Jones Lab tested this by examining the development of TLE in mice following an initial epileptogenic insult using EEG, and measuring their pattern separation memory function using behavioral tests and c) measuring the ability of their isolated dentate gyrus tissue to perform pattern separation.
In parallel, in collaboration with Bruce Hermann’s lab, the Jones team tested pattern separation memory in human patients in the UW-Madison Epilepsy Monitoring Unit. They found that both mice and humans with epilepsy had problems with pattern separation memory compared with control subjects, and in mice, there was a relation between their preclinical epileptiform brain activity (e.g., interictal spikes), their memory deficit and the ability of their isolated dentate gyrus tissue to perform pattern separation.
Summary:
This work shows that both humans and mice with TLE have deficits in a specific type of memory that probably involves the dentate gyrus. The mouse work further shows that these deficits may be related to both preclinical EEG activity such as interictal spikes and to malfunction of the dentate gyrus circuit itself. Translationally, the most interesting thing is that humans and mice that are *at risk* for TLE both show a specific type of memory deficit that depends on the dentate gyrus. Therefore, testing for this specific memory deficit could predict which individuals are most likely to develop TLE after an initial insult, such as a head injury. It is currently not possible to predict who will go on to develop epilepsy after an initial insult. Such a memory test is noninvasive and inexpensive. This test was given to patients in the Epilepsy Monitoring Unit on a laptop in about 15 minutes per patient as part of their standard neuropsychiatric workup upon being admitted to the unit. So, this is a potentially very workable cognitive screen that might predict future risk for epilepsy.
Antoine’s hypothesis is that pathology in this brain area is simultaneously responsible for seizures and for learning/memory deficits that accompany epilepsy. Antoine’s work showed that hippocampal circuit computations are pathologically altered in mice with epilepsy and that corresponding memory problems occur in both mice and human patients with epilepsy. Antoine earned his PhD in May 2018 and is now continuing his research as a postdoctoral fellow at the University of Chicago.
Two papers from his PhD thesis are in final stages of peer review and a third paper will be submitted in Spring of 2019.
BioRxiv preprints available at https://doi.org/10.1101/107706 and https://doi.org/10.1101/421479.
Postdoctoral fellow Jesse Pfammatter has also been blazing a trail in a new direction for the Jones lab: high throughput analysis of electroencephalogram (EEG) data for seizures, NonConvulsive Epileptiform Events (NCEEs, e.g., interictal spikes, etc) and sleep. Patients with epilepsy often complain of disrupted sleep, and sleep loss is one of the most common triggers for seizures, suggesting a vicious cycle that may lead to disease progression. The reasons behind these relations are not at all understood, largely because quantitative analysis of EEG records for sleep and epileptiform events is incredibly time-consuming and costly. Furthermore, seizures are relatively rare (often much less than one per day), whereas NCEEs happen very often (hundreds per day) but are almost never quantified because of time and cost bottlenecks. Jesse has developed machine learning algorithms that can detect NCEEs exactly as precisely as expert humans, but about 300 times faster. The ability to rapidly and quantitatively measure NCEEs opens entirely new avenues for a mechanistic understanding of the relations between epileptiform events and sleep states, and how these relations evolve during epileptogenesis. The translational goal of this work is to establish novel non-invasive electrographic biomarkers for early diagnosis of risk (e.g., after an initial insult such as head trauma or febrile seizure) and prediction of response to therapy.
Jesse recently published one paper on these methods in PLoS ONE and has another one in final stages of peer review: https://doi.org/10.1371/journal.pone.0207158 and https://doi.org/10.1101/309146
2015 and 2018 Grant: Looking for the “Master Regulator”
With the support of a $100,000 two-year grant from Lily’s Fund, Avtar Roopra, PhD and his team are exploring a novel genetic pathway that may be involved in the development of epilepsy.
Although scientists are beginning to understand how changes in the brain contribute to the progression of epilepsy, they know little about what drives and coordinates these changes. Avtar wants to know if there is a “master regulator” that coordinates the process of epileptogenesis.
Using a computer algorithm to sift through data from 11 independent labs, Avtar has determined that a specific complex of proteins may orchestrate many of the changes in the epileptic brain. Drugs have already been developed to target this complex. Avtar’s goal is to see if these same drugs might stall the progression of epilepsy.
During this last funding period Roopra Lab has published in 3 major publications and validated their principle prediction outlined in the initial Grace Grant proposal. The algorithm, MAGIC, that was developed by Roopra and made the EZH2 and IKAROS predictions, has now been peer reviewed and published in PLoS Computational Biology[1]. The Epilepsy Microarray Consortium dataset that was the input for MAGIC and is a resource used by the entire field is also published in Science Data[2]. Finally, the finding that EZH2 is a major driver of gene changes in epilepsy – the focus of our previous Grace Grant award – is published in PLoS One[3].
Their initial proposal was based on MAGIC analysis and Grace Grant funds were requested to 1) validate that IKAROS is indeed induced in epilepsy and 2) targeting IKAROS will be therapeutic. We are excited to report that the first of these 2 aims is completed.
The next step will be to define the cell types in which IKAROS is induced. This will be accomplished via immunofluorescence using NeuN, GFAP and iba1 antibodies to colocalize IKAROS. When they can identify the cell type they will be in a position to knockdown the gene via vial approaches as outlined in the original application.
The Roopra Lab is in the process of determining efficiency of Lenalidomide targeting of IKAROS and plan on performing drug efficacy tests within the next 3 months.
1 Roopra A. MAGIC: A tool for predicting transcription factors and cofactors driving gene sets using ENCODE data. PLoS Comput Biol 2020; 16: e1007800.
2 Dingledine R, Coulter DA, Fritsch B, Gorter JA, Lelutiu N, McNamara J et al. Transcriptional profile of hippocampal dentate granule cells in four rat epilepsy models. Sci Data 2017; 4: 170061.
3 Khan N, Schoenike B, Basu T, Grabenstatter H, Rodriguez G, Sindic C et al. A systems approach identifies Enhancer of Zeste Homolog 2 (EZH2) as a protective factor in epilepsy. PLoS One 2019; 14: e0226733.
We see a robust increase in the levels of a novel ‘ Master’ regulator that starts one day after status epilepticus and continues past the 10 day time point. This is exciting because prior work by others has shows that a drug that blocks this Master is a very promising anti-epileptic drug. Recently, it has been found that in various cancers, this drug can slow disease progression and it works by causing degradation of the Master. Thus we believe that the Master’s up-regulation in epilepsy contributes to the disease and that this anti-cancer drug is protective because it targets the Master for degradation.
Avtar’s unique research project, funded with a $100,000 grant from Lily’s Fund, focuses on the hypothesis that a master regulator molecule exists in the brain and is responsible for orchestrating all the detrimental changes that occur in people with epilepsy. He and his team used “big data” to help identify this elusive molecule.
“We have a good handle on what it is – most likely a molecule that was originally discovered as a master regulator of body plan formation in flies! We have found that in humans, it controls the majority of changes that occur over time in epileptic brains.”
So what does that mean to those with epilepsy? Avtar’s lab successfully tested a drug that blocks the regulator and this drug appears to prevent the unwanted gene changes in brains after seizures. On the heels of this very exciting finding, they are now running additional experiments with the same drug, to see if it suppresses spontaneous seizures that are the hallmarks of epilepsy.
“There is one thing we had not anticipated when we first proposed studying the master regulator: Our drug only had to be administered for three days after the seizure. It looks like that will be sufficient to prevent the gene changes occurring for life. More work will be required to really test this idea,” says Avtar. “If this project continues at this pace of discovery, we may have a drug that doesn’t just stop seizures, but prevents the actual progression of the disease.”
The Spark Grant from Lily’s Fund has lived up to its name, serving as the catalyst for significant additional funding from other outside sources.
Based on the data gathered with support from the $100,000 award from Lily’s Fund, Avtar’s lab secured two R21 federal grants from NIH – each worth $275,000. They were also able to secure a highly competitive challenge award from Citizens United for Research in Epilepsy (CURE), worth $250,000. CURE gives out only one Challenge Award worldwide each year, and Avtar says they could not have done it without Lily’s Fund.
Lily’s Fund Boosts Promising New Avenue of UW Epilepsy Research
(UW-Madison SMPH News Release, Jan 28, 2015)
Madison, Wis. – Leveraging data from around the world, Avtar Roopra thinks he may have found a common genetic link among the many variations of epilepsy. That link, he hopes, can take the shape of a target to stop the progression of epilepsy.
The “shot in the arm” that will move the research to the next level is a two-year, $100,000 grant Roopra received on Saturday, January 24 at Lily’s Luau, a local event put on by Lily’s Fund for Epilepsy Research. For him, the grant from Lily’s Fund means that he can pay salaries and purchase reagents and compounds needed for this project.
A research consortium of nearly a dozen labs across the globe embarked on a concerted effort to understand the mysteries of epilepsy, using various models of rat epilepsy to study. Each model had strengths and weaknesses, and seizures were induced in a variety of ways depending on the model.
But Roopra, a professor of neuroscience at the University of Wisconsin School of Medicine and Public Health, is interested in what the models all have in common.
“The data we get with this grant will set the groundwork for a much bigger grant which will allow us to really tear this problem apart.”
– Avtar Roopra
“Understanding what’s common in all models may tell us something very basic about epilepsy, regardless of how the epilepsy starts,” said Roopra. “With that as a backdrop, we got ahold of all the data these labs generated through all their different models. We measured the level of gene expression — the amount of a gene’s activity in the brains of these animals — in these large electronic data sets.”
The Roopra lab used the genetic data from each disease-model rat as well as control animals, analyzing the 28,000 active genes in the brain of each rat. What they discovered was that several protein complexes, “master regulators” that turn genes on and off, were controlling nearly all of the genes that change after a seizure is induced.
According to Roopra, the first seizure a person has does not mean epilepsy. That seizure is simply an insult that may cause gene changes, perhaps making the brain more prone to seizures in the future. Therefore, targeting the changes in the brain could have better outcomes compared to treating the symptom of seizures.
With this early data in hand, the Roopra lab now plans to test its hypothesis that these two or three master regulator proteins drive all the changes seen in epilepsy. The plan is to try to stop these regulators, and perhaps stop the gene changes in the brain that happen after a seizure to stop the brain from becoming epileptic.
“In reality, to really get to the bottom of this, we’re probably looking at three to five years of solid work by several people who will do nothing else but study these master regulators, and we’re talking about hundreds of thousands of dollars, perhaps even a million dollars in funding,” said Roopra. “To convince the National Institutes of Health to give us that kind of resource, they need to be convinced that we’re on to a real good lead, and so for that, we need more preliminary data to make that case.”
Roopra said the Lily’s Fund grant is will function as a much-needed primer.
“The data we get with this grant will set the groundwork for a much bigger grant which will allow us to really tear this problem apart. That’s why Lily’s Fund and others are so important now more than ever, when funding at the federal level is so tight. They allow us to prime the pumps of data generation so that we can get enough data to make the case to federal agencies.”
While continuing to underwrite postdoctoral and graduate research fellowships and other epilepsy research projects at the UW School of Medicine and Public Health, Lily’s Fund volunteers designed a new grant program to respond quickly to emerging research opportunities.
“This special grant represents the convergence of two inspiring trends,” said Anne Morgan Giroux, founding member of Lily’s Fund for Epilepsy Research. “First, we have generous donors who have really stepped up to the plate to support epilepsy research. That puts us in a position to support entrepreneurial scientists at UW-Madison who want to explore new frontiers. It’s grassroots philanthropy fueling innovative research.”
Lily’s Fund is an all-volunteer organization that celebrates and supports epilepsy-related research at UW-Madison. The organization has raised over $800,000 since its inception in 2006. The seventh annual Lily’s Luau, held at UW-Madison’s Union South, netted a record $145,000.

2014 Grace Grant: Using HD-EEG to Locate Seizures and Pathways
Dr. Giulio Tononi, UW-Madison neuroscientist and psychiatrist, received the inaugural two-year Grace Grant to see if high-density electro encephalograph (HD-EEG) technology can be used to identify the focal point of seizures in the brain, as well as calculate the seizure’s pathway.
Locating that point of origin is critical for patients preparing for brain surgery. The traditional scalp EEG does not provide enough detail, so neurosurgeons must rely on intracranial EEG (electrodes placed directly on the brain itself). This invasive approach increases the risk of infection and other complications.
HD-EEG technology may offer an accurate way to find the source of seizures, without the invasive approach. This method might also predict the pathways of the seizures and how they move across the brain, an under-studied area of epilepsy.
“If high-density EEGs can be used to accurately locate the focal point of seizures, physicians would have an entirely new way to plan for brain surgery. For epilepsy patients, this could minimize the number of tests and avoid invasive monitoring that requires multiple surgeries,” said Tononi.
“Over the next two years, we hope to study at least 20 patients, examining how seizures spread through the brain’s cortex. This is a very novel approach – one that might yield insights on the pathophysiology of seizures,” said Tononi.
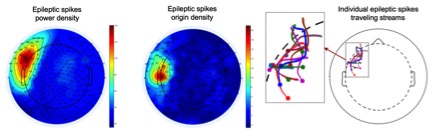
Since receiving the first ever $100,000 Grace Grant from Lily’s Fund, Giulio Tononi and Rama Maganti were able to acquire high-density EEG recordings in 20 patients with focal epilepsy at the UW Epilepsy Monitoring Unit. Each recording lasted between 24 and 48 hours, producing a data set that allowed researchers to study how epileptic spikes travel in the brain from their point of origin.
“Our preliminary data show that epileptic spikes do indeed travel across the brain, in a pattern that is consistent across spikes within the same patient, but different from one patient to the other. We plan to use this data to write a first manuscript and to submit a grant to NIH,” says Giulio.
While analyzing the same data acquired with support from Lily’s Fund, the team also uncovered new links between epileptic activity and changes in brain activity during sleep.
“We found that patients with epilepsy show a deeper sleep than healthy controls, and that the depth of sleep is proportional to the amount of seizure activity during wakefulness preceding sleep – as if it was compensating for it. In contrast, epileptic spikes during sleep seem to decrease the efficiency of sleep,” says Rama.
Based on the team’s findings, epilepsy scientists may be able to identify preferential routes of epileptic activity and target those areas of the brain in surgery. Additionally, the new data regarding sleep activity, and how epileptic spikes disrupt sleep, suggest that epilepsy therapy should aim at not only preventing seizures, but also quelling interictal spikes.
Building upon this work at UW-Madison, future epilepsy research might focus on the similarity between epileptic spikes and the spread of seizure activity leading to loss of consciousness. Further studies should also compare results obtained using high-density EEG recordings to those obtained using intracranial recordings.
“We have preliminary data in one epileptic patient, showing that this comparison is feasible. These results open a whole new line of research for our team and others to improve the pre-surgical planning of patients with focal epilepsy,” says Rama . “Knowing how epileptic activity moves across the brain in individual patients could allow more accurate surgical techniques and better outcomes for the patient.”
During 2014, the Tononi lab focused on using high density EEG to locate seizures and their pathways. The question: Can HD-EEG locate the source of epileptic seizure for pre-surgical planning? Using this advanced technology, can scientists predict how seizures might move across the brain?
To date, the team has successfully recorded HD-EEGs in 15 patients with refractory epilepsy who were undergoing pre-surgical evaluation. The researchers successfully captured 27 seizures and 1500 spikes during these extended recordings. Using special software to decode massive amounts of data captured by the HD sensor arrays, the lab has detected single events such as spikes, the location of seizure onset, and the pathways the seizures followed.
Using methods developed at the Tononi lab, patients with more than 30 epileptic spikes (11 of the 15 subjects) are being analyzed to assess how individual EEG events travel over the cerebral cortex. These analyses will help scientists better understand how epileptic activity spreads from the seizure onset zone to the rest of the cortex.
The on-scalp HD-EEG data are then compared to traditional intracranial (within the skull) recordings in the same patients to validate results.
Additionally, the team evaluated a distortion of sleep homeostasis (slow-wave, non-REM sleep) in regions of the brain associated with epilepsy onset, and found additional abnormalities.
Due to the success of their recordings and analysis, the team is now in the beginning stages of preparing the first manuscript of this study. They are also applying for an NIH grant to further study epileptic spikes as travelling waves.
Giulio Tononi, UW-Madison neuroscientist and psychiatrist, is working with a two-year Grace Grant to see if high-density electro encephalograph (HD-EEG) technology can identify the focal point of seizures in the brain and calculate the seizure’s pathway. Locating that point of origin is critical for patients preparing for brain surgery. HD-EEG technology has been used extensively in sleep research, but its application in a clinical setting has been limited, due to the tremendous amount of information coming from 250 electrodes simultaneously. Giulio has developed proprietary software that can help interpret that data, in ways that might yield important breakthroughs for epilepsy patients. He and his collaborators have completed HD-EEG recordings in 4 patients, all of whom had epileptic activity captured. They will continue recruiting patients, followed by some careful analysis of the resulting data.